Implementing Value-Based Healthcare for Success
After reading this article, you will be able to define the various value-based payment models and list the facilitators and barriers to a successful program.
SUMMARY:
Value-based healthcare aims to provide patient-centered care by aligning provider incentives with outcomes.
This is a complex challenge, with heterogeneous and inconsistently reported results.
Achieving success in implementing value-based healthcare depends on recognizing and managing the factors that promote or impede its effectiveness
COMMON PAIN POINTS
Management: Lack of consistent leadership
Data: Inconsistent, patient data siloed across systems
Model Complexity: Lack of transparency on incentives to providers
Patient Engagement: Patient perspective not taken into consideration
Regulatory: Unstable regulatory environment
REVIEW
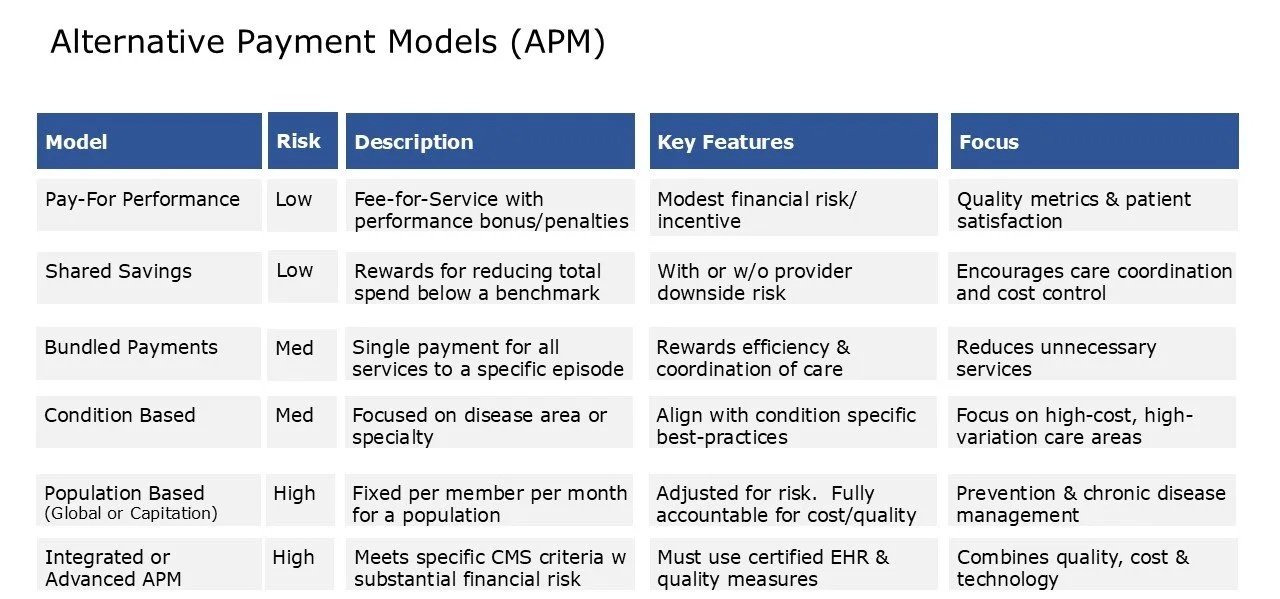
ALTERNATIVE PAYMENT MODELS:
Traditional fee-for-service payment models, pay providers for each service.
Value-Based payment models shift from volume to value, and link payments to quality, outcomes and efficiency.
There are several types of value-based payment models. The most common are:
Pay for Performance – Fee for service plus bonus payments for quality.
Shared Savings – Providing care at a cost below a certain benchmark for a patient population.
Bundled Payments – Payment for services related to a specific episode of care.
Population-Based – Global payment to manage the overall care for a defined population.
OUTCOMES:
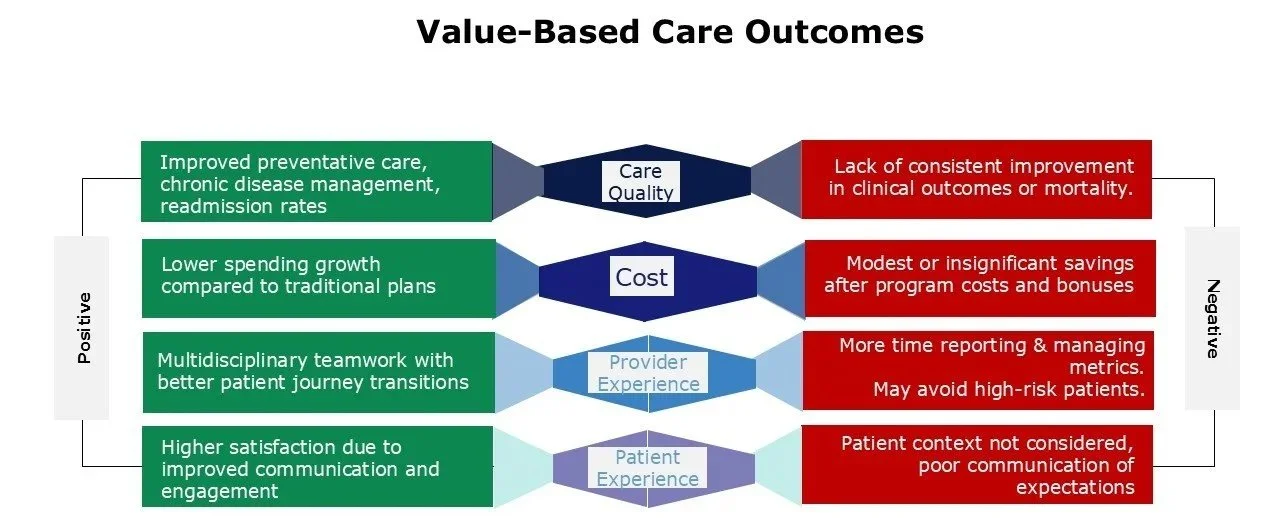
Conflicting results have been reported with value-based programs based on:
Program design
Patient population evaluated
Parameters measured
Outcomes Reported
Care quality
Cost savings
Provider Experience
Patient Selection and Experience
FACILITATORS:
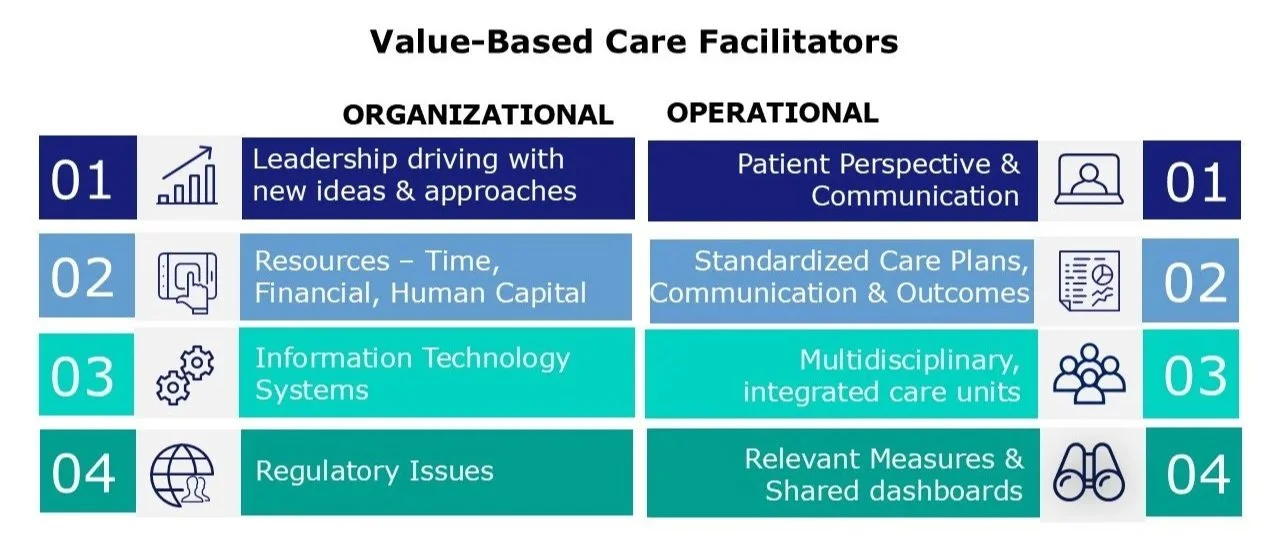
Many factors can help facilitate a value-based care program. The main areas which help are:
ORGANIZATIONAL FACTORS:
Leadership: The most consistently reported facilitator; bringing new ideas, continuously improving and evolving approaches over time.
Resources: Those necessary for appropriate design of program, and improved implementation. Includes financial, time and human capital
Tailored Business Plan: Define the vision and strategy. Provide a structured, clear, and goal oriented process.
Organizational Structure: Convert to a disease oriented organization. Most systems remain in silos and is difficult to associate outcomes with costs and patient continuity.
Communication and Education: Clinical staff and Patients.
Legal & Regulatory Updates
OPERATIONAL FACTORS
Multidisciplinary team: Engaging all clinicians involved in the care of the patient over time.
Care Transition Integration: Ensure seamless patient management throughout patient journey.
Standardization of Outcome Measures: Data transparency and benchmarking. Real-time data sharing mechanisms. Accessibility of data and outcomes.
The Patient Perspective: Include the patient’s point of view to align patient experience with how the team provides care.
Robust Clinical Dashboards
Facilitate Communication between providers and patients.
BARRIERS:
Insufficient funding
Resistance for providers to adopt value-based programs – reliance on fee-for-service model
Lack of IT infrastructure
Lack of multidisciplinary care approach in organizational structure
Lack of data collection process
Misaligned financial incentives
Lack of resources for adequate data collection & analysis
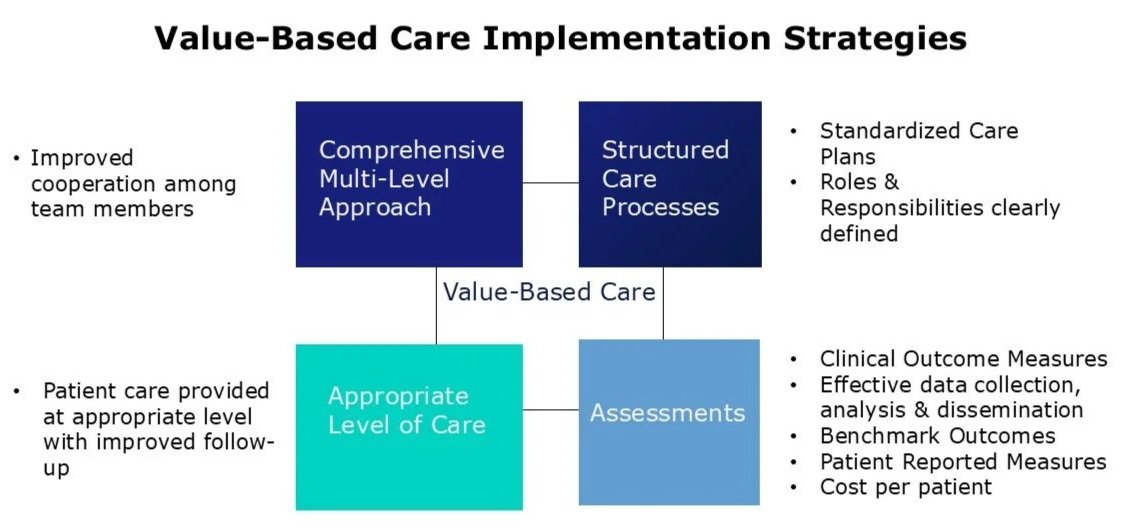
VALUE-BASED CARE IMPLEMENTATION STRATEGIES
Comprehensive, multi-level care approach: Multidisciplinary team of care delivery across patient journey care transitions.
Care provided at the appropriate level of care with improved follow-up
Improved structured care processes: Standardized Care Plans, mapped out care processes with roles and responsibilities clearly established.
Assessments: Patient population level dashboards and reports, Clinical outcome measures, Dissemination of data in an efficient manner, Benchmark outcomes between sites, Trending data, Patient-reported measures, Costs.
CONCLUSIONS:
Value-Based care aims to deliver high-quality, patient-focused care at greater value.
These programs have not uniformly achieved the desired goals.
A successful program necessitates an understanding of the various models, risks, approaches, and ways to overcome the known challenges.
value-based care programs come in several different forms.
Successful value-based programs have unique challenges with inconsistent RESULTS reported.
Identifying and managing the relevant factors for success are critical for effectivenss
Do not leave this to chance, - let’s have a brief chat to discuss your unique situation