The Future of AI in Chronic Care Management
After reading this article, you will be able to discuss the value of combining AI with multiple data streams in chronic care management and current challenges.
SUMMARY:
Artificial Intelligence (AI) will transform chronic care disease management (CCM).
The value of AI is combining multiple data streams to provide timely risk assessments and early warning prompts to better coordinate care plans between patients and clinicians.
The key concerns center on patient engagement for self-care and workflow integration.
Validation of clinical effectiveness remains missing.
CHRONIC CARE CONSIDERATIONS:
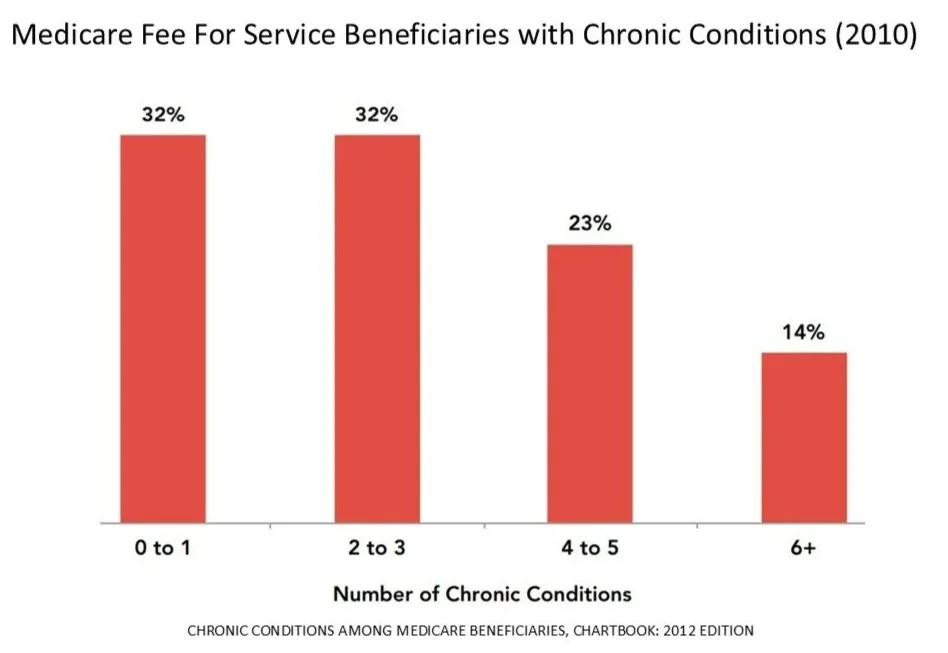
In 2023, approximately 194 million (76.4%) of U.S. adults reported at least 1 chronic disease.
130 million (51.4%) reported multiple chronic conditions
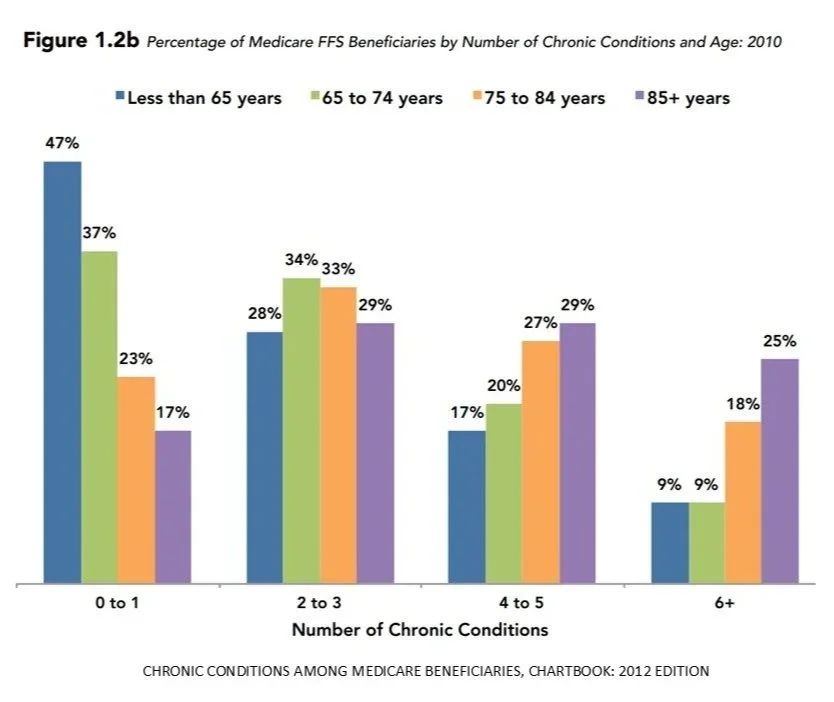
The number of chronic conditions increases with age.
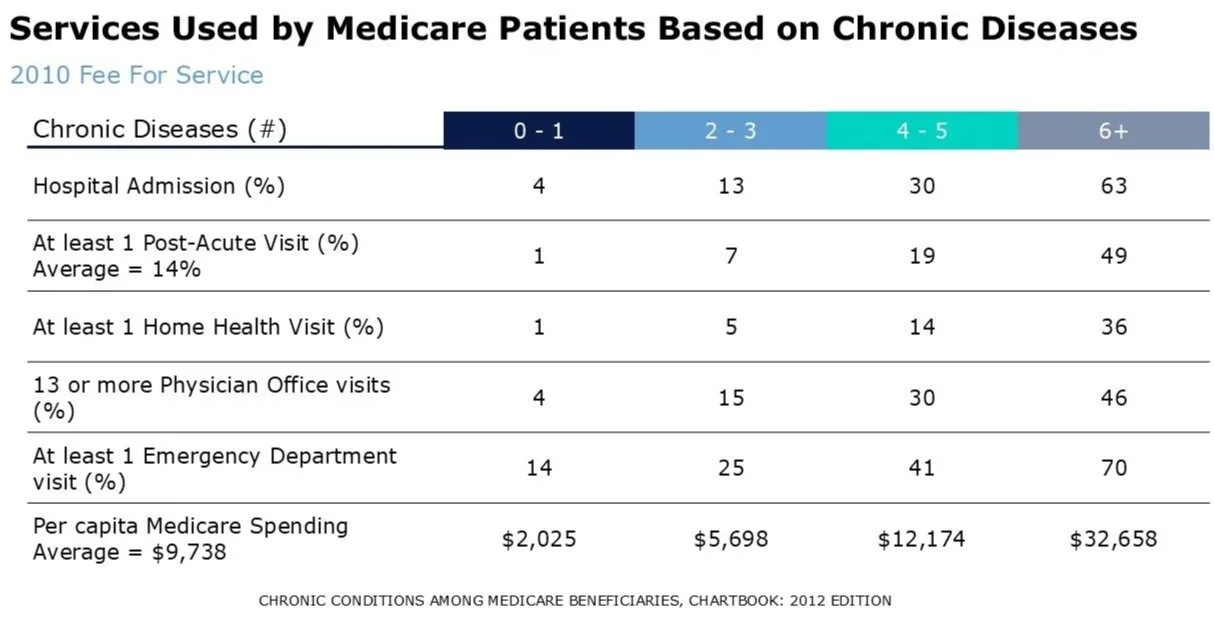
Use of healthcare services increases with increased number of chronic conditions.
Self-management by patients is a valuable task to improve health, quality of life, and reduce costs.
Self-management efforts focus on:
Medication adherence
Lifestyle modifications
Diet
Exercise
Symptom identification and management
Active involvement in treatment decisions
ROLE OF AI:
The rapidly evolving advances in digital health and AI have provided tools to identify patterns and predict individual responses.
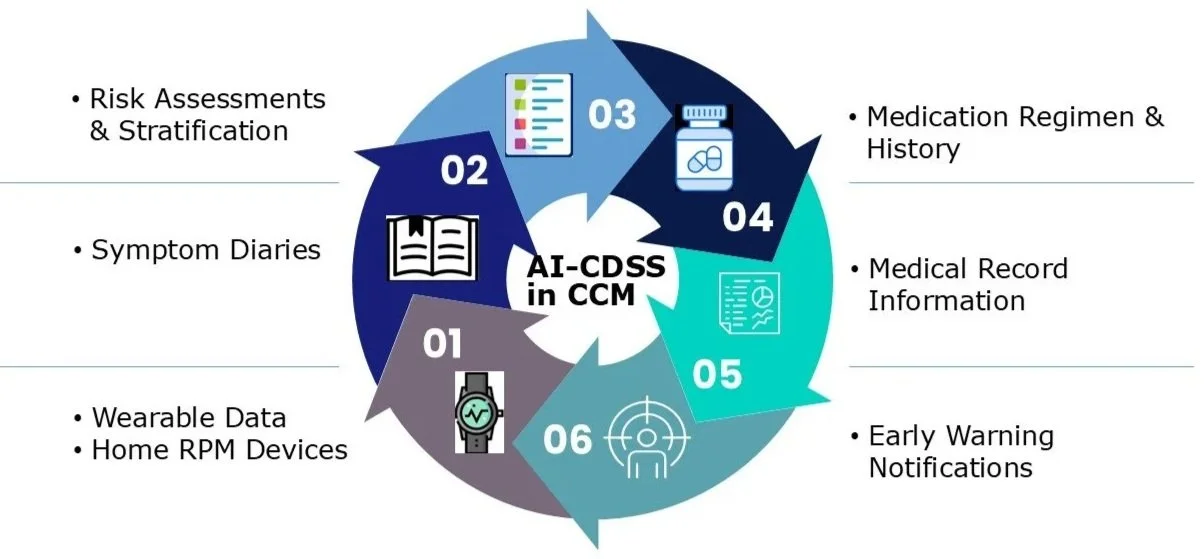
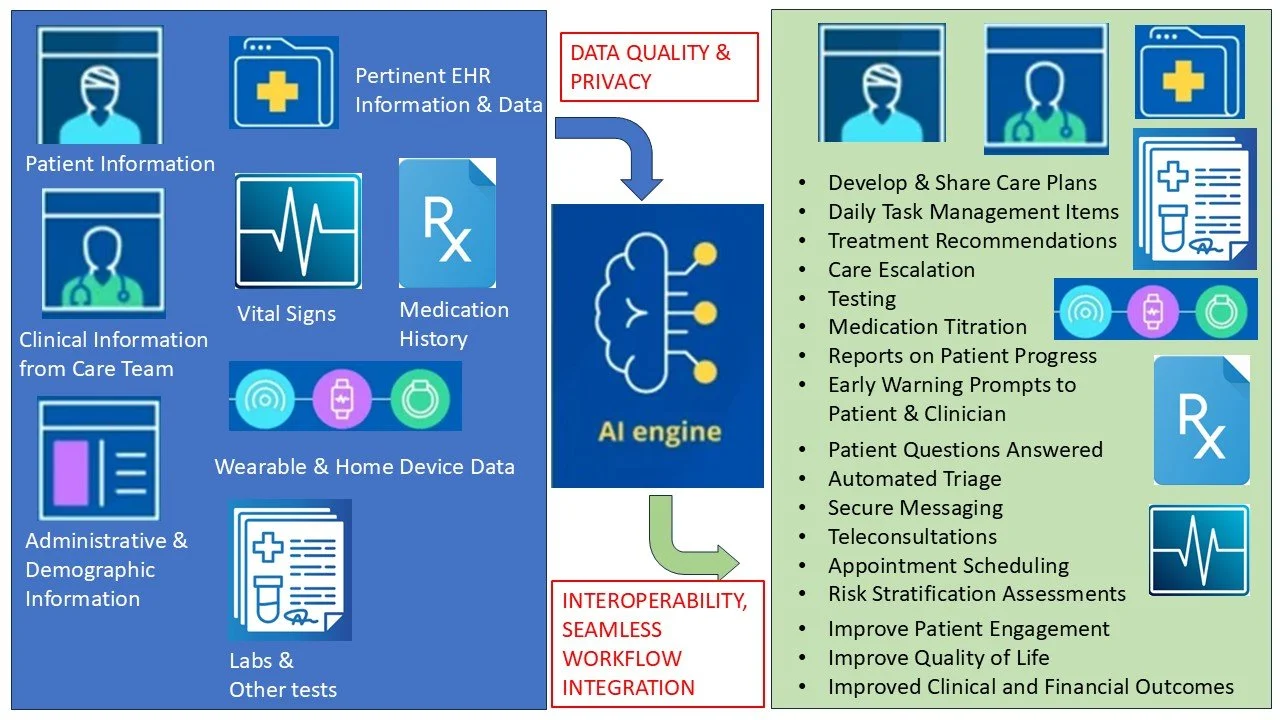
Unlike previously passive clinical decision support tools (CDSS), AI-CDSS can couple continuous multiple data sources (i.e., physiologic data from wearables, home devices, symptom diaries, medication history, EHR data to provide timely risk assessment and stratification and early warnings.
The goals of AI-CDSS in CCM are to:
Improve coordination of information between patient and clinician
Share jointly developed care plans
Use digital health solutions (secure messaging, teleconsultations, etc) for triage, escalations, and follow-up
Improve between face-to-face visits gaps
The strongest components of AI-CDSS in CCM are: monitoring and predictive analytics, producing:
Near real-time risk assessment
Early actionable warning prompts
Success of AI-CDSS for CCM depends on:
Patient engagement
Workflow integration
Data quality
Interpretability
Seamless integration into routine care
AI-CDSS CHALLENGES IN CCM:
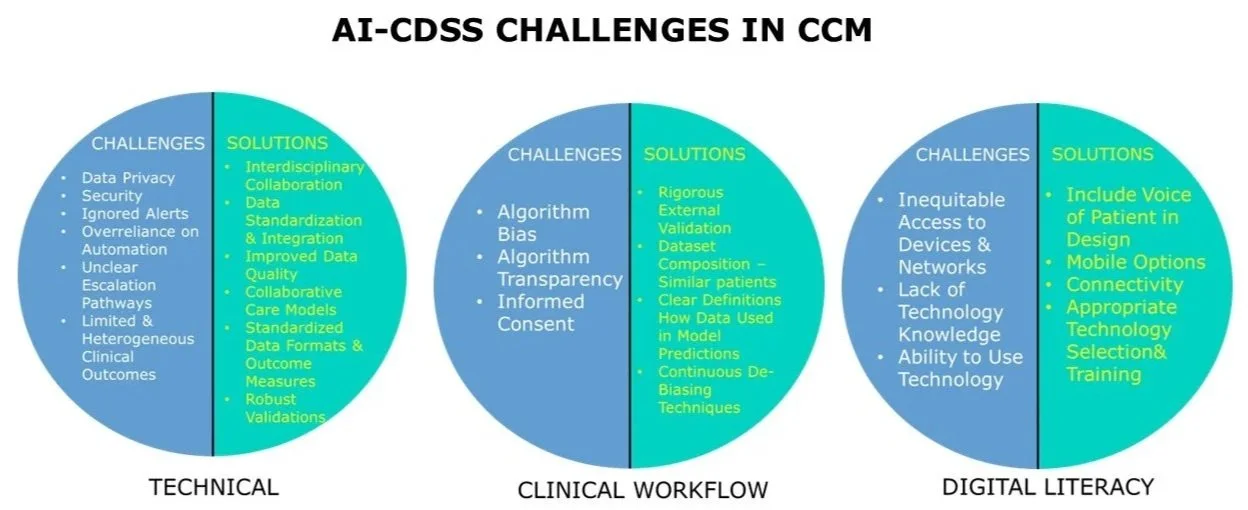
TECHNICAL:
Data privacy
Security
Ignored alerts
Overreliance on automation
Unclear escalation pathways
Limited & heterogeneous clinical outcomes
Solutions:
Interdisciplinary collaboration & training
Data standardization and integration
Improved data quality
Collaborative healthcare models
Standardized data formats and outcome measures
External robust validation across patient populations, establishing clinical effectiveness
INCORPORATING AI-CDSS INTO CLINICAL WORKFLOWS:
Algorithm bias
Algorithm transparency
Informed consent
Solutions:
Rigorous external validation is necessary
Dataset composition – ensure patients are similar and grouped together
Clearly define how data inputs are used in model predictions
Ongoing de-biasing techniques, even after the system is in use
DIGITAL HEALTH LITERACY AND ACCESSIBILITY
Inequitable access to devices and/or network
Lack of knowledge in digital technology (patient and provider)
Ability to use technology
Solutions:
Voice of the patient included in designing the care model
Mobile options
Connectivity
Appropriate selection and training of the technology used
FUTURE DIRECTIONS & OPPORTUNITIES FOR AI-CDSS IN CCM:
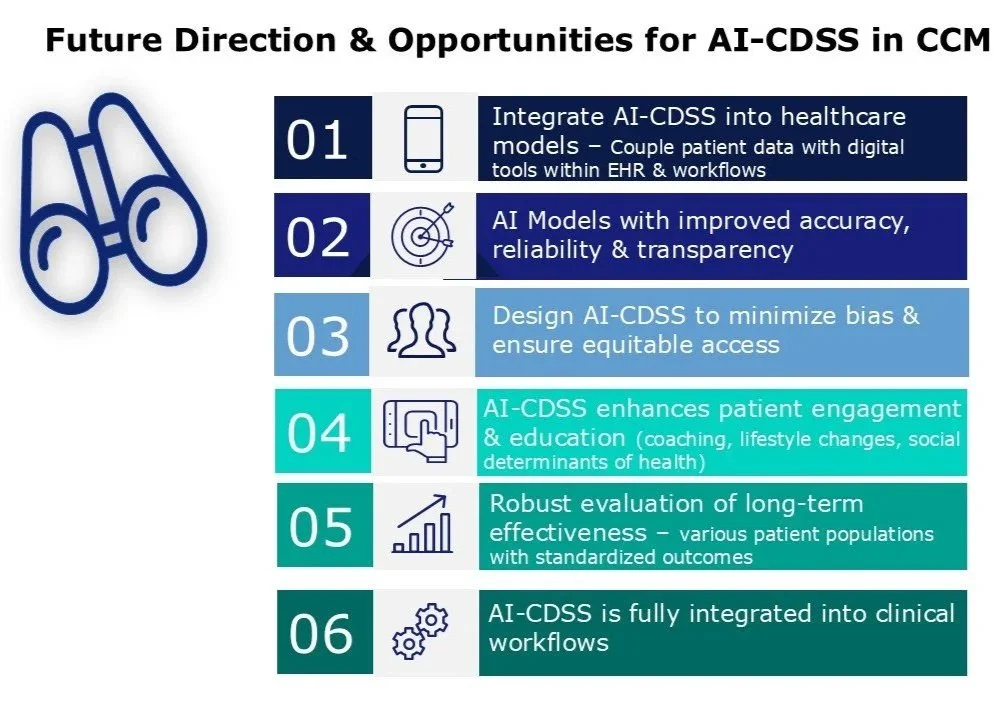
Integration of AI-CDSS into the current healthcare system care models
Interoperable platforms coupling patient data from wearables and digital tools within the EHR and clinical workflows.
AI models with improved accuracy, reliability, and transparency
Attention to ethically designed AI-CDSS to minimize bias and ensure equitable access
Evolution of AI-CDSS to enhance patient engagement and education.
Integrate data from devices, diet, and daily activities
Provide real-time coaching
Reminders to encourage sustained lifestyle changes
Robust evaluation of long-term effectiveness, with standardized outcome measures across various patient populations.
Implementation of AI-CDSS fully integrated into clinical workflows
CONCLUSIONS:
AI-CDSS for CCM will play an increasing role in the future by coupling collected data from various devices with clinical notes, medication history, and social determinants of health.
Rigorous evaluations of long-term clinical effectiveness in various patient populations are needed.
Clinical oversight will be needed to combine the AI-CDSS CCM results with risk stratification, early warnings, diagnostic and screening to appropriate patient support.
Chronic diseases place a large burden on the global healthcare system.
Supporting patient self-management of multiple chronic diseases over a lifetime is a significant challenge.
The rapidly evolving digital health technologies and AI offer substantial potential to address these challenges.
AI in chronic care can enable personalized interventions, greater monitoring, predictive notifications, and improve patient engagement in self-care.
Initial results are encouraging, but challenges remain with data privacy; overreliance on automation; limited clinical outcome data; poor integration into clinical workflows; and data literacy and access.